IUDs 101: Is an Intrauterine Device the Right Birth Control For You?
When it comes to birth control, you have a lot of options. One of those are IUDs, or Intrauterine Devices. But what exactly is an IUD? Is it better than taking birth control pills? We believe knowledge is power, so we’re breaking it down for you with our IUD 101 blog.
Learn more about IUDs, their pros and cons, and what you should consider when deciding on your birth control options. Informed decisions are the best decisions!
What does IUD mean?
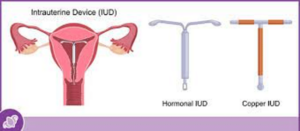
IUD stands for intrauterine device. Broken down, this means, inside (intra) of the uterus (uterine) device. It is a plastic, T-shaped device that is designed to fit inside of the uterus.
What are IUDs used for?
IUDs are most commonly used for contraceptive purposes (to prevent pregnancy), but they can sometimes also be used to help with heavy or abnormal menstrual bleeding.
I’ve heard IUDs can cause bad side effects. Is that true?
The types of IUDs used today are different from those used decades ago. Unfortunately, IUDs have gotten a bad reputation due to devices from the past that caused bad side effects and complications. Fortunately, these old devices are no longer available, and current IUDs are very safe! All procedures carry some risks and having an IUD placed is the same. The risks associated with IUD placement today are small when they are placed by experienced women’s health providers, such as our Care Team at Diana Health. Before you choose to go forward with an IUD insertion, your provider will review and discuss the risks and benefits with you so that you can make a fully informed decision.
Are there non-hormonal IUDs? What about IUDs with hormones?
Although most IUDs look similar, they are not all the same. There are two kinds of IUDs currently available in the U.S.:
Non-hormonal: The Paragard IUD uses copper in order to have its effect on the uterus. No hormones are used with this IUD and it is effective for up to 12 years.
Hormonal: Mirena, Kyleena, Liletta, and Skyla are all examples of hormonal IUDs. These IUDs use progestin, a hormone similar to progesterone that the female body makes, that is released from the IUD in order to have its intended effect. These IUDs are effective for 3-8 years depending on the brand that is used.
How does an IUD prevent pregnancy?
Hormonal IUDs thicken your cervical mucus, which makes it difficult for sperm to get inside of the uterus. Also with hormonal IUDs, eggs are sometimes prevented from being released from the ovaries too. Non-hormonal IUDs, such as a copper IUD, repel the sperm with the copper, making it almost impossible for the sperm to make it past the IUD.
Since the sperm and egg are prevented from meeting in both instances, pregnancy is prevented.
Like with all birth control, there is a small chance that a pregnancy can still occur. However, IUDs are extremely effective methods of contraception or birth control that last for several years. In fact, they are over 99% effective at preventing pregnancy. In comparison, ideal male condom use for contraception is about 98% effective; however, typical use is only about 87% effective.
How is an IUD placed in the uterus?
Before inserting an IUD, you and your healthcare provider should discuss your health history and preferred method of contraception. Your healthcare provider will tell you about the pros and cons of various types of contraception, the different types of IUDs, options (including doing nothing), the pros of having the procedure (eg. contraception, possibly decreased bleeding), and the potential risks of having the procedure (e.g., very small risk of still getting pregnant, pain, bleeding, infection, risk of the IUD falling out, etc).
You will sign a consent form if you decide to proceed with an IUD placement. You may or may not be given medication to take prior to the procedure.
Your provider will typically conduct a pelvic exam so that they can determine the size and position of your uterus. Next, a speculum (the metal or plastic device that is used during pap smears to help the healthcare provider see your cervix) is placed in the vagina and opened, allowing the cervix (opening of the uterus/womb to the vagina) to be visualized. The cervix is cleaned with betadine or another solution to decrease the risk of infection. This usually involves a large swab being wiped across the cervix.
Next, a device may be placed on the cervix to help hold it in place during the procedure and another tool may be used to find out how large the inside of the uterus (endometrial cavity) is, in order to help with proper placement. Sometimes if the opening to the womb is very small, dilators may be used to help it open enough for an IUD to be placed. Using a small tube that goes through the cervix and into the endometrial cavity, the IUD is placed with its “arms” aligned with the tube.
Once in the uterus, the IUD is pushed out so that its “arms” can open and the IUD can stay in the proper place in the endometrial cavity. Next, the small tube is removed and the string that is attached to the end of the IUD is cut so that just a couple centimeters remains outside of the cervix, in the top of the vagina.
The speculum is removed and the procedure is done! The total time for the procedure varies by person, but typically takes less than 10 minutes.
Is having an IUD placed painful?
It is normal to have some discomfort and cramping during the procedure. However, your healthcare provider will walk you step-by-step through the procedure that typically only takes a few minutes. After the procedure you may continue to have some cramping and light bleeding. If you have severe pain, heavy bleeding, a fever, or other problems, reach out to your healthcare provider immediately as this is not typical. If you’re concerned about pain during the procedure, talk with your provider to see if they recommend taking something for discomfort prior to your insertion, such as ibuprofen or acetaminophen.
When does the IUD need to be removed?
IUDs are “good” and effective for a certain amount of years, but it can depend on the type of IUD and brand of IUD. When you have your IUD placed, your provider will let you know when it needs to be removed. If you decide that you want to try to get pregnant or if you decide that you want your IUD out at any time prior, you can book a visit for an IUD removal. IUDs can be removed at any time, based on your needs and preferences.
How are IUDs removed?
IUDs are typically easy to remove through a quick procedure in our practice. First, the speculum is placed in the vagina. Next, the string is grasped by a device that allows the strings to be held tightly. Then the string is pulled and the arms of the IUD go upwards as the IUD is pulled out through the cervix. That’s it! It may cause a little cramping but most women tolerate it very well.
For more information on IUDs, visit https://www.cdc.gov/reproductivehealth/contraception/index.htm
If you are considering an IUD for yourself, or simply want to discuss all of your contraception options, book a visit with the Diana Health Care Team! We’re here to help empower you with the knowledge and resources you need to make the right decision for you!
Share This Post